What is Prolapse?
When it comes to pelvic floor health, there are so many topics that rarely get discussed — and I’m doing my best to change that. Women deserve to have shame-free conversations about what’s going on in their bodies, especially during those pregnancy and postpartum seasons when everything seems to be constantly changing.
Almost every pelvic floor diagnosis is more common than you think!
You’re not alone, and there is a way to treat your symptoms and strengthen your body for the new seasons ahead. Today, I want to take the lid off the conversation on pelvic floor prolapse (POP), a condition that affects up to half of all women over the course of their lives.

What is Pelvic Floor Prolapse (POP)?
POP occurs when one of your pelvic organs drops out of position. No, this does not mean your organ has fallen out of your body — it simply means the organ is pressing into the wall of the vagina.
This generally happens due to weakened muscles and ligaments in your pelvic floor.
Pelvic floor prolapse is a general term that refers to the pelvic organs, including your vagina, uterus, bladder, urethra, small intestine, or rectum, shifting out of their regular position and pressing into your vaginal wall. Sometimes, POP can affect multiple organs, either because one has dropped and placed pressure on another, or because multiple organs have dropped due to pelvic floor dysfunction.
The symptoms of POP are not uniform — not every woman will have every symptom! But if you’re experiencing any of the following, seek out a pelvic floor specialist to help you diagnose what’s going on.
- Pressure, fullness, or discomfort in your pelvis
- Seeing or feeling a bulge in your vagina
- Urinary incontinence or bowel dysfunction
- Finding it difficult or impossible to insert tampons
- Pain and pressure during sex
POP can happen suddenly, but more often, it occurs over time.
Prolapse is actually diagnosed and “graded” based on severity, and there are several specific types of prolapse depending on which of your organs are affected. For this reason, it’s important to see a pelvic floor specialist right away for an accurate diagnosis — plus, it may help you solve the problem with conservative treatment before it worsens.
Who does POP affect?
Pelvic floor prolapse often affects women in postpartum, but you don’t need to have birthed a child to experience POP.
Let’s quickly look at the numbers:
- Roughly two thirds of women who have given birth present with anatomical evidence of POP
- Majority of women with evidence of POP are asymptomatic (no symptoms)
- Around 40% of all women ages 45-85 years have evidence of POP
- Only 12% of these women experience symptoms
- Lifetime risk for surgery in women with POP is 11.1%
Prolapse can happen due to aging or hormonal changes, high-intensity workouts or heavy lifting, disease or genetic disorders, and countless other reasons.
Here are several risk factors:
- Parity (the # of times you’ve given birth, more births=higher risk)
- Vaginal delivery
- Age (increased age=increased risk)
- BMI (increased BMI=increased risk)
- Baby’s birthweight
- Family history
- Chronic constipation
- Use of forceps or vacuum during delivery
As I mentioned earlier, there is no shame in this! It’s a very common condition, and treatment is available for POP symptoms that are causing you pain or discomfort.
How can POP be diagnosed and treated?
Pelvic Floor PT
One of the most important parts of managing prolapse and its accompanying symptoms is to manage your intra-abdominal pressure.
Intra-abdominal pressure is the pressure within your abdominal cavity. If you place too much pressure down into your pelvic floor, you can imagine it will increase that downward pressure of your pelvic organ(s) into your vaginal walls therefore worsening your prolapse.
Strengthening the muscles and ligaments of your pelvic floor can help to alleviate POP symptoms and give your organs the support they need to stay in place. You might also benefit from pelvic floor muscle release depending on your symptoms!
When you visit my office (or your local pelvic floor PT!), you’ll get a full explanation of which exercises will help and why. We’ll do some pelvic floor work during your appointment, and you’ll get some “homework” for you to continue strengthening your pelvic floor right at home!
Here are a few exercises you might receive from your pelvic floor PT as homework!
Here are some examples of what your pelvic floor PT may work on to improve your prolapse:
- Diaphragmatic breathing
- Releasing pelvic floor tension
- Improving pelvic floor muscular endurance or strength
- Improving pelvic floor muscle coordination
- Increasing lower body strength
- Addressing proper standing and sitting posture
- Improving rib and thoracic mobility
Lifestyle Modifications
Sometimes, POP can occur due to excessive coughing, heavy lifting, the straining that comes with constipation, poor posture, or other lifestyle factors.
Maintaining proper posture with your ribs stacked over your hips is one of the most beneficial things you can do on a regular basis to help improve your prolapse symptoms.
You can also work on your prolapse by avoiding or reducing constipation by: staying hydrated (think half of your body weight in ounces of water per day…at least!), investing in a squatty potty, and ensuring you are eating an adequate amount of fiber on a daily basis.
If any of these factors are contributing to your diagnosis, your pelvic floor specialist can help you find relief through modifying some of these mitigating factors.
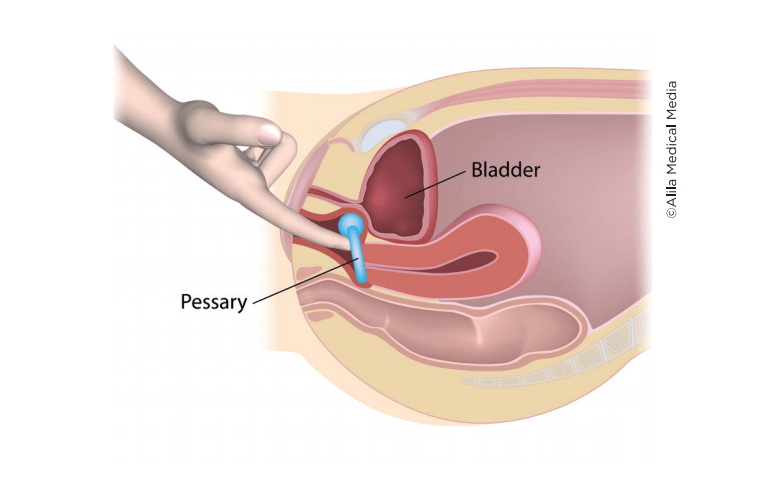
Pessary Device
If your pelvic floor and organs need some extra support as you heal, a pessary device can be a simple solution!
Essentially, this is a removable ring, designed to be worn in the short term while you recover from POP and strengthen your muscles and ligaments again.
Multiple types are available, so your doctor or pelvic floor specialist should be able to help you decide which type is best for your situation — they may even be able to fit you for a pessary right in their clinic!
Typically, pessary devices are used for 3-6 months, but of course, you’ll need to consult your medical professional to get the right treatment plan for you.
Surgery
If conservative treatment options are not enough to treat your POP, surgery to fix prolapse is an option. I would always recommend at-home or in-clinic treatment as a first resort, but sometimes, surgery is the best option!
There are lots of factors to consider — for example, if you have postpartum POP and you hope or plan to get pregnant again in the future, you should postpone surgery until after your last birth.
Prolapse can recur in subsequent pregnancies, and I never want my clients to face an unnecessary surgery. Like any procedure, you would also need to consult your surgeon about the potential risks, as well as which surgical method is best for your specific case.

Need more help?
If you’re experiencing pelvic floor dysfunction due to giving birth, aging, or injury, remember that this isn’t your fault, and you don’t have to face it alone.
I became a pelvic floor PT because I wanted to help women learn about their bodies, heal them, and strengthen them for the long haul.
My Movement Through Early Postpartum rehab program will help you optimize your postpartum healing by learning to manage your intra-abdominal pressure, improve pelvic floor and full body strength, and reduce pelvic floor tension through daily workouts and educational videos.
Check out the free demo now!
And if you are looking for more personalized care, make sure to schedule an appointment with your local physical therapist. You can find one here!
[…] for prolapse, diastasis recti, and other common postpartum […]
[…] Rectal prolapse (check out my “What Is Prolapse?” blog post here) […]
[…] I’ve written about this condition in detail on the blog, but here’s a quick list of symptoms you may be experiencing with POP: […]