Pelvic Floor 101: The “Health Class” Most Women Never Got
When was the last time someone actually explained your pelvic floor to you?
If you’re like most women, the answer is probably never, even though your pelvic floor plays a role in some of the most important (and most everyday) parts of your life: bladder and bowel control, sexual comfort and pleasure, core strength, pregnancy, birth, and postpartum recovery.
And if you’ve ever dealt with leakage, constipation, painful sex, pelvic pressure, or that vague “my body feels different now” feeling after having a baby – this is your reminder that you’re not broken. Most women simply weren’t given the education they deserved about how this part of the body works.
This is your pelvic floor 101 class: the anatomy and functions explained in a way that actually makes sense, plus we’ll discuss what can go wrong, and what to do about it in a practical, non-overwhelming way.
What Is the Pelvic Floor?
Your pelvic floor is a group of muscles that sits at the base of your pelvis like a supportive bowl, hammock, or sling.
It extends:
- from your pubic bone in the front
- to your tailbone in the back
and out to your sit bones on either side
So instead of thinking of it as one single muscle, picture it as a layered support system. Your pelvic floor has three distinct layers, and each layer can contribute differently to symptoms. That matters because pelvic floor dysfunction isn’t always simply “weakness,” sometimes it’s tension, poor coordination, or a mix of several things.
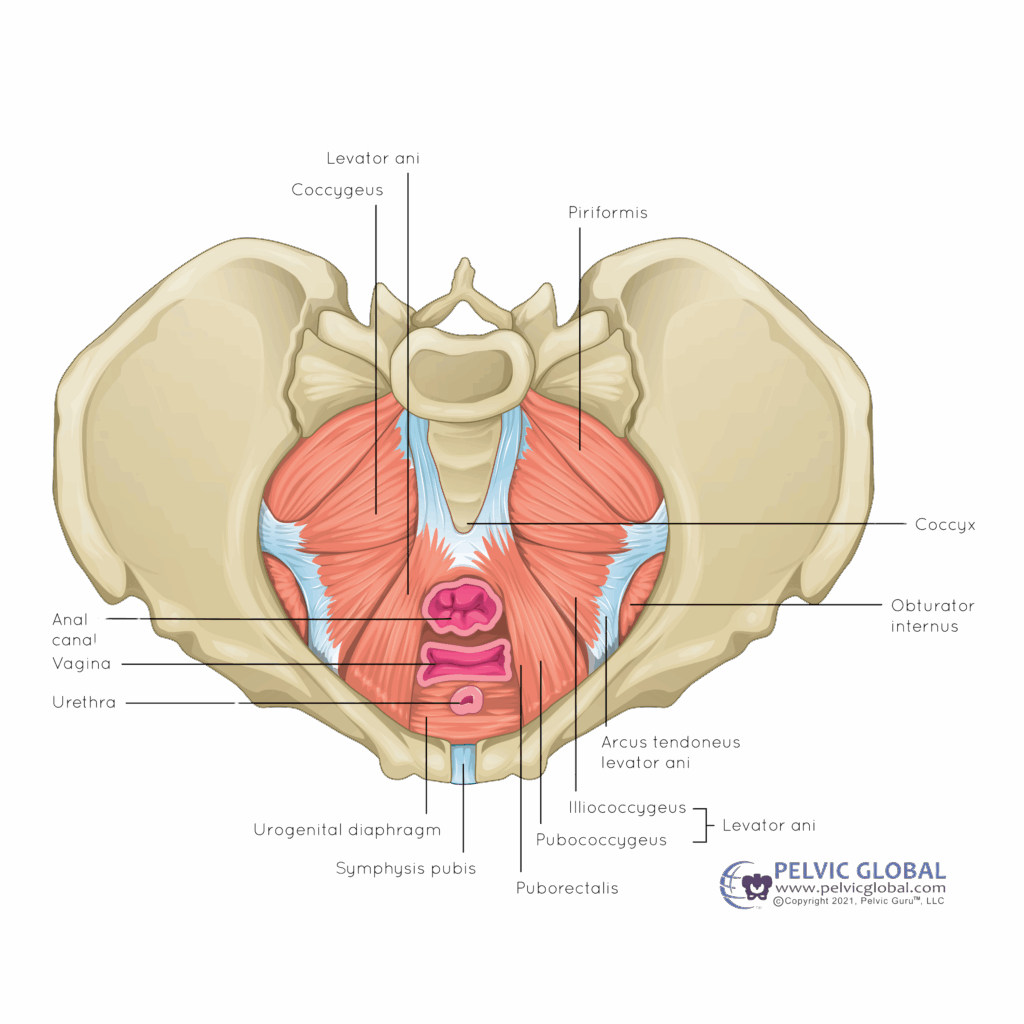
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)
Your pelvic floor doesn’t work alone
One of the most helpful ways to understand the pelvic floor is to stop thinking of it as separate from the rest of your core.
Think of your body like a soda can:
- The top of the can is your diaphragm (your main breathing muscle)
- The bottom of the can is your pelvic floor
- The sides of the can are your abdominals and obliques
- The back of the can is your lower back muscles
Together, this system helps your body manage pressure inside your abdomen and creates stability for movement whether that’s lifting weights, picking up a toddler, carrying a pregnancy, or simply getting through daily life without pain or leaking.
When this system isn’t coordinating well, that’s often when symptoms show up.
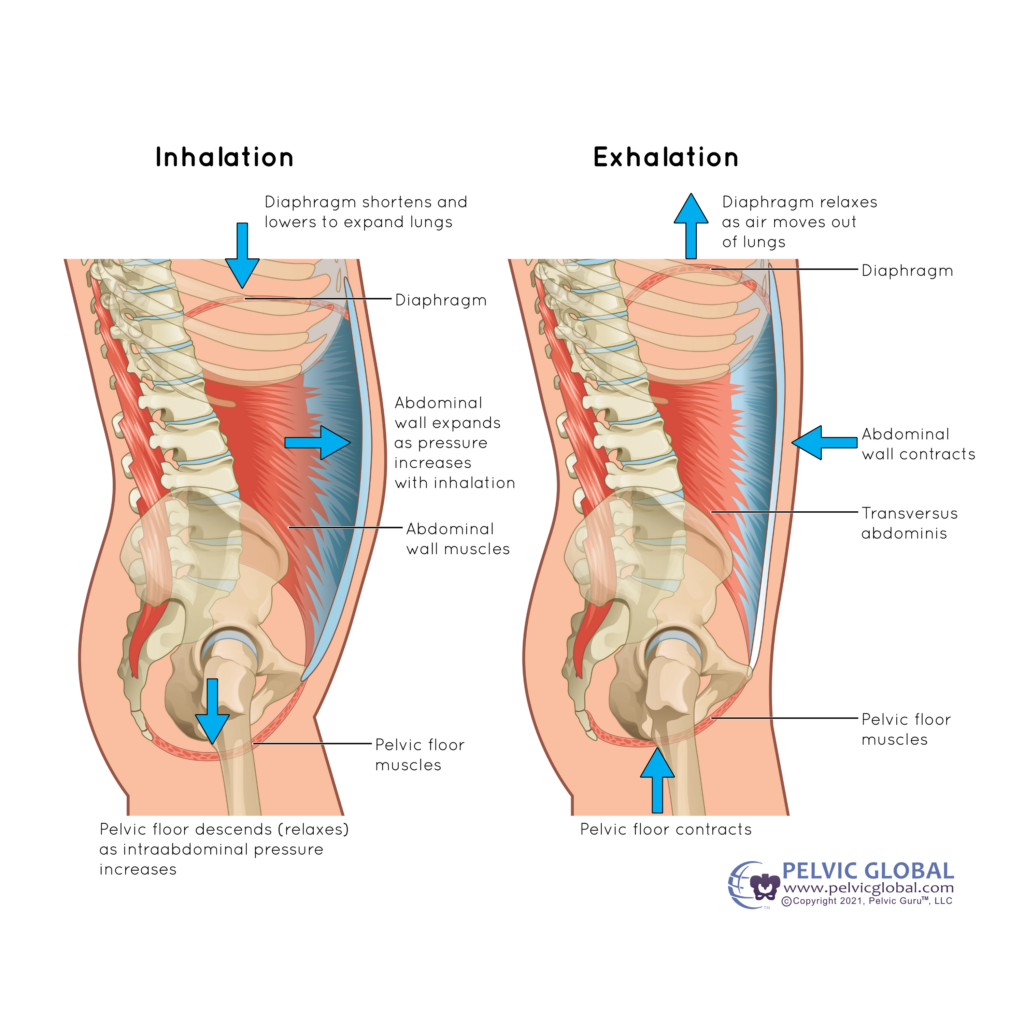
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)
What Does the Pelvic Floor Do? The “Five S’s”
A simple way to remember the key jobs of your pelvic floor is the Five S’s:
- Support
- Stability
- Sphincter control (bladder and bowel control)
- Sexual function
- Sump pump (circulation support)
Let’s break those down in a way that’s easy to apply to real life.
1) Support
Your pelvic floor helps hold up your pelvic organs, like your bladder, uterus, and rectum, as if they’re resting in a supportive bowl.
This function becomes especially important during pregnancy because your growing baby and uterus sit directly above the pelvic floor, increasing pressure on those muscles over time. That pressure doesn’t automatically mean something will go wrong, but it’s one reason pelvic floor symptoms can appear or worsen during pregnancy, especially later in the third trimester.
If you’ve ever felt pelvic heaviness or pressure during pregnancy or postpartum, this “support” function is often part of the conversation.
2) Stability
Remember the soda can analogy? Your pelvic floor acts as the base of your inner core system.
When it coordinates with your diaphragm, abdominals, and lower back muscles, it helps stabilize your spine for:
- everyday movement
- carrying and lifting
- strength training
- picking up your child (over and over and over)
This is why pelvic floor health is not just “a pelvic thing.” It’s a whole-body thing. When your pelvic floor isn’t doing its part (or is doing too much), your body may compensate in ways that show up as low back pain, hip pain, or core instability.
3) Sphincter Control (Bladder + Bowel Control)
Your pelvic floor muscles wrap around the openings in the pelvis, particularly the urethra (where urine comes out) and the rectum (where stool passes).
To function well, your pelvic floor needs to be able to do both:
- contract to close those openings when needed
- relax to allow urine and stool to pass
This is where a lot of women get surprised: pelvic floor symptoms are not always caused by weakness. Tension matters too.
For example:
- If your pelvic floor is very tight around the urethra, it can make it harder to start your urine stream or fully empty.
- If your pelvic floor is tight around the rectum, it can contribute to constipation, straining, or the feeling that you can’t fully empty your bowels.
Constipation is one of the most common pelvic floor-related issues women deal with—often without realizing the pelvic floor is involved at all.
4) Sexual Function
Your pelvic floor also wraps around the vaginal opening, contributing to:
- arousal
- vaginal comfort
- sensation and orgasm
If your pelvic floor is too tight, it can feel like the vaginal opening is “closed off,” making penetration uncomfortable or painful which is something many women experience, especially early postpartum.
On the flip side, if the pelvic floor is very weak, it can decrease the intensity of orgasm for some women because orgasm relies partly on rhythmic pelvic floor contractions.
This is one of those topics that should be more normalized: pelvic floor changes can affect sex, and that doesn’t mean anything is “wrong” with you. It usually means your pelvic floor needs support, healing, and the right kind of retraining.
5) Sump Pump (Circulation + Swelling Support)
This one is less commonly discussed, but it’s important.
As your pelvic floor muscles contract and relax, they help return blood and lymph back toward your heart acting like a sump pump for circulation.
When the pelvic floor is tight or under constant pressure, it can restrict flow in the vessels of the pelvic region. During pregnancy, when blood volume increases and pressure in the pelvis is higher, this can contribute to swelling and discomfort.
One example is vulvar varicosities, which are basically varicose veins in the vulvar region. Think “spider veins,” but in the pelvis. They can be uncomfortable, heavy, and sometimes shocking if you’ve never heard of them before, but they’re often connected to the pressure and circulation changes that happen in pregnancy.
What Can Go Wrong? Common Types of Pelvic Floor Dysfunction
Now that you know what the pelvic floor is supposed to do, let’s talk about what can happen when those functions get disrupted.
Most pelvic floor dysfunction falls into one of three patterns:
- Tightness
- Weakness
- Poor coordination
And here’s the key: you can have more than one at the same time.
1) Pelvic Floor Tightness
A tight pelvic floor is one that struggles to relax and lengthen when it needs to.
Symptoms can include:
- pain with intercourse
- constipation or difficulty passing stool
- trouble starting the urine stream
- pelvic, hip, or low back pain
- tension you can’t quite “turn off”
And if you’re pregnant and preparing for birth, this matters: your pelvic floor needs to be able to relax, lengthen, and get out of the way as your baby moves through the birth canal. When the pelvic floor is very tight, it can make that process feel more challenging, not because your body is failing, but because the muscles are resisting a job that requires openness.
(That’s also why “just do kegels” is not universally helpful advice in pregnancy. Some women need strength. Many need relaxation and coordination. And plenty need both.)
2) Pelvic Floor Weakness
Weakness is often what women assume all pelvic floor issues come from especially when leakage is involved.
Weakness can show up as:
- leaking with coughing, sneezing, laughing
- leaking with running or jumping
- difficulty controlling gas or stool (less common, but possible)
In many cases, weakness means the pelvic floor isn’t strong enough to close the sphincters against sudden pressure – like the pressure spike that happens when you cough or sneeze.
But again: weakness isn’t the whole story for everyone. Which brings us to the third pattern.
3) Poor Coordination (Not Too Tight, Not Too Weak)
This is one of the most overlooked causes of pelvic floor symptoms.
Sometimes the pelvic floor has decent strength and isn’t excessively tight, but it doesn’t activate at the right time or in the right sequence with the rest of your core.
Example: If you need your pelvic floor to contract quickly right before a cough or sneeze, but it contracts a beat too late, leakage can happen even if the muscle isn’t “weak” in a traditional sense.In other words, the issue isn’t always strength. Sometimes it’s timing.
How to Improve Pelvic Floor Health (Without Overcomplicating It)
If you’re wondering what to do with all this information, here are three simple, foundational starting points.
1) Start With Awareness
Awareness is not fluffy, it’s functional.
Learning:
- where your pelvic floor sits
- where the openings are (urethra, vaginal opening, rectum)
- what the pelvic floor is supposed to do
…can be genuinely transformative.
Many women start improving their pelvic floor health simply because they finally understand what they’re feeling.
2) Connect Pelvic Floor + Breath
Your diaphragm (breath) and pelvic floor are a team.
A helpful pattern to practice:
- Inhale: pelvic floor gently relaxes/descends
- Exhale: pelvic floor gently lifts/engages
This helps regulate pressure inside the “soda can,” improves coordination, and teaches your pelvic floor how to move through its full range – both relaxation and contraction.
3) Strengthen With the Rest of Your Body
Your pelvic floor doesn’t function in isolation, so your rehab shouldn’t either.
The best long-term results come from improving pelvic floor function while strengthening:
- hips
- glutes
- deep core
- posture and breathing mechanics
Because the pelvic floor is foundational strength for your entire body, especially during pregnancy and early postpartum.And yes: this is why your pelvic floor is so much more than kegels.
If You Want Guided Support
If you’re pregnant and want pelvic floor–integrated workouts to carry you through every stage of pregnancy, Movement Through Pregnancy is a 37-week strength training program that integrates pelvic floor function into every workout, so you’re not guessing what’s safe or effective.
If you’re postpartum and ready for a structured plan that supports healing, Movement Through Early Postpartum is a 12-week program designed to rebuild pelvic floor and core function progressively, aka, a step-by-step rehab roadmap for early recovery.
The goal isn’t to “bounce back.” The goal is to rebuild from the inside out, so you can feel strong, confident, and supported in your body again.
If this post helped you understand your pelvic floor in a new way, keep it bookmarked and continue following along for more pregnancy, postpartum, and pelvic floor education.