What is Diastasis?

If you’re pregnant or planning to be, you’ve probably heard stories from moms about abdominal separation and wondered how much you should worry about it. You may have heard it called “mom belly” or “split abs,” but this common condition is officially called diastasis recti.
There’s plenty of information about it online — but a lot of that information makes it seem scary. Instead, I’m to help you understand exactly what diastasis recti (commonly abbreviated as DR) is, how it can be treated, and how to take care of your core if you do develop it. Let’s take a peek at the facts and alleviate any fears you may have! I promise, a DR diagnosis is not as scary as you think.
What is “the core”?
You’ve undoubtedly heard countless health and fitness professionals talk about the important role your core plays in overall strength, but how exactly is it defined? Think of your torso as a can of soda. Your diaphragm sits at the top, and your pelvic floor is at the bottom. These two hold everything between them in place. The “sidewalls” of this soda can are made up of your abdominal muscles in the front and lower back muscles in the back.
Some people mistakenly believe that your core consists of just your abdominal muscles. But actually, all of these pieces work together to keep everything within your core where it belongs, from your internal organs to a growing baby when you’re pregnant! Your diaphragm, pelvic floor, abdominals, and lower back muscles all combine to maintain proper intra-abdominal pressure in the belly. Without that proper pressure, various dysfunctions show up in the core. This can present as low back pain, pelvic pain, diastasis and more.
What are your abdominal muscles?
With DR specifically, your abdominal muscles are affected. Your abs are so much more than the “six-pack” we sometimes reference in muscular people – they run deep into your core and stabilize your body. And no, you don’t need a six-pack to have a strong core! There are four main abdominal muscle groups:
- Transverse abdominis: This is the deepest muscle in your core. It’s responsible for stabilizing the spine.
- Internal obliques: Sitting deep in your sides above your hips, these muscles bend and rotate the trunk of your body.
- Rectus abdominis: These are the ab muscles that we think of when we say “six pack!” They’re on the front of your stomach, and they bend the trunk of your body forward.
- External obliques: These muscles are on top of your internal obliques, but they serve much of the same purpose, bending and rotating the trunk of your body.
What happens when someone gets diastasis?
What is normal?
Let’s start by saying this – EVERYONE technically has diastasis recti, not just women who are pregnant or postpartum. Your rectus abdominis muscle (the large muscle in the front of your core) is actually split into two halves, which are connected by a thin band of tissue called the linea alba. So the rectus abdominis muscle is split into two for every one, male or female!
The linea alba allows our rectus abdominis muscle to stretch for two important reasons.
- Pregnancy – Without this thin tissue, the abdominal musculature would not be able to stretch to accommodate your growing baby!
- Breathing – Your abdominal musculature expands as you inhale and shrinks as you exhale, so without this thin tissue it would be extremely difficult to take a full breath!
Now that you know the gap between the two halves of your rectus abdominis muscle is purposeful and important for function, let’s look at some normal ranges for linea alba width in women who have never been pregnant.
This study measured linea alba width at 3 different points in 150 women ages 20-45 years who had never been pregnant.
- Xiphoid 0-31mm
- 3cm above the belly button 1-35mm
- 2cm below the belly button 0-31mm
From this study you can see that there is a large variation in what naturally occurs in women who have never even had children! So yes – most women are born with an anatomical “gap” and the goal is not to completely close the gap.
What about diastasis during pregnancy?
Diastasis recti is a perfectly normal condition that develops during many pregnancies, and it’s also often found in postpartum women to a lesser extent. I just want to pause and say that again: developing DR during pregnancy is totally normal! It’s actually considered a functional adaptation, allowing your abdominal wall to create space for your growing baby. At least 2 in 3 women develop DR by the 3rd trimester of their pregnancies.
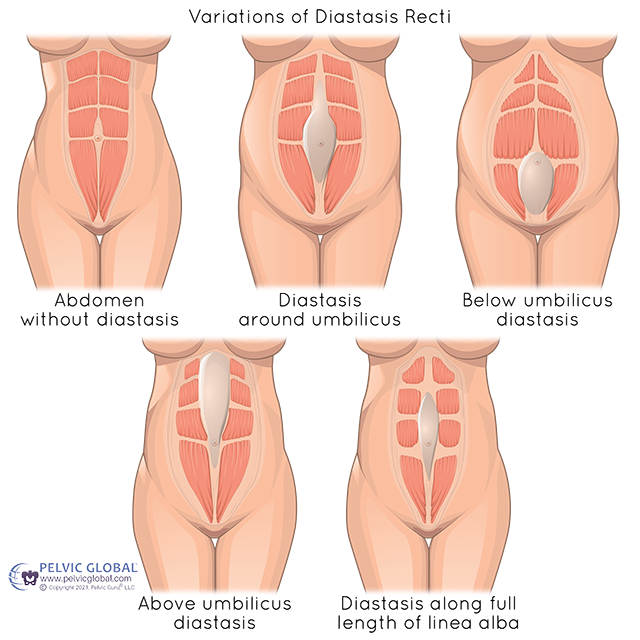
Image used with permission from Pelvic Guru®, LLC www.pelvicglobal.com
Most textbooks and research studies define DR as a linea alba width that is greater than 2cm, however we know from the above information that there is a large variation in normal widths ranging from 0 to 3 cm in women who have never had children!
When you develop DR during pregnancy, the tissue is stretched, which can create a gap between the two halves of the rectus abdominis muscle. Because of that connective tissue being stretched, contracting your core with DR makes the gap deeper or causes a bulge in your stomach.
While it’s normal for the linea alba to stretch during pregnancy, you do want to avoid excessive stretching that leads to permanent tissue damage. This can happen with core exercise or any full body exercise that places too much of a demand on the tissue and causes “coning.” DR typically will resolve within 6-8 weeks postpartum in which your linea alba width will return to its baseline width before pregnancy, but many women still have symptoms at 6 months.
However, it is important to note that the emphasis is less on the width of the gap and more on the function of your abdominal muscles. You want to make sure both halves of the rectus are communicating well with one another and you are able to control your intra-abdominal pressure.
So if you’re not seeing a quick return to your pre-pregnancy abs, you are not the only one! Make sure to schedule an appointment with a pelvic floor physical therapist no later than 6 weeks postpartum to ensure you are taking the proper steps to facilitate healing of your DR.
How do I know if I have DR?
If you see a pelvic floor PT for postpartum rehab, they’ll test you for it! You can also perform a self-check. To do so, you’ll use your fingers to gently press at your belly button, above, and below. Then, contract your core muscles to feel for the width and depth of the gap between the halves of your rectus abdominis. You can have separation in one portion of the linea alba but not the entire thing – there’s a lot of variety in where DR presents.
If you do feel a gap, don’t be alarmed! Many women never return to their pre-pregnancy gap width, but they still have full abdominal function. The “textbook” definition of a normal width is about 2cm, but we know that naturally occurring width can vary greatly among individuals, so instead focus on your function and symptoms. If you are experiencing pain, loss of functionality, incontinence, or other symptoms, schedule a pelvic floor PT visit.
I have DR. How can I get help?
If you’ve been diagnosed with DR during pregnancy, the best thing you can do postpartum is start working with a pelvic floor PT right away! When you address this issue within the first 6 weeks postpartum, you can ensure you are utilizing proper breathing techniques. You can also begin functional exercises that will help reduce the abdominal gap and restore proper function of your core muscles.
Unresolved diastasis can lead to a bulge of the belly that makes some women still look pregnant, so there are aesthetic reasons for wanting to minimize stretching and tissue damage along the way. However, there are important functional purposes for treating postpartum DR as well! Diastasis is associated with weaker abdominals, which can lead to low back pain, hip pain and pelvic floor dysfunction. If you need to find a pelvic floor provider in your area, this is a great place to start.
Diastasis Myths and Fears Debunked
After reading this post, I hope you feel more prepared to handle this aspect of pregnancy and postpartum life! Some abdominal stretching during pregnancy is completely normal, but there are definitely ways to help reduce that stretching — and to ensure you aren’t accidentally causing excessive damage to your abdominal muscles. It’s important to stay active, even if (or especially if) you have DR, but moving in safe ways will minimize potential damage.
Want to keep your abs safe and strong throughout your pregnancy? My Movement Through Pregnancy program was designed to help you find safe ways to move and strengthen your body throughout every trimester. You’ll find pregnancy safe circuits that target the core and pelvic floor — like this one. There are even educational modules about DR!
If you’ve already had your baby, you’re not out of luck. My latest program, Movement Through Early Postpartum, walks you through the first 6 weeks of postpartum recovery. It’s designed to help you heal your core in a progressive manner, teaching your abdominals how to work together again and reducing the linea alba gap. You’ll also find educational modules to help you along the way.
DR doesn’t have to ruin your core forever. You can find strength, safe movement, and functionality through every stage of pregnancy and postpartum life! Cheering for you, mama.