Does Breastfeeding Impact Your Pelvic Floor?

If you’re a new mom who plans to nurse, you’re likely expecting the changes that come with beginning to breastfeed. Chafing, latching problems, pumping, clogged ducts — it all comes with the territory. But what you may not expect are some postpartum changes in your pelvic floor, even after you’ve healed from giving birth. Yep, breastfeeding and pelvic floor health are tied. I’m here to tell you how so that you know just how to navigate these changes with ease.
What is the Pelvic Floor?
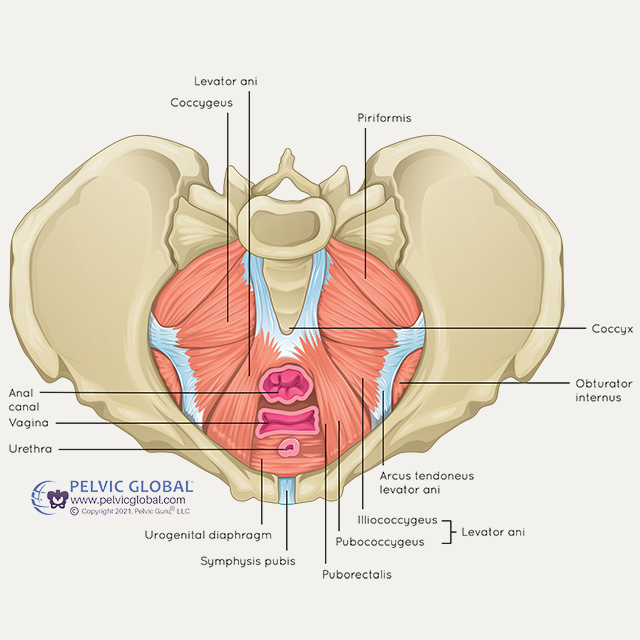
Before I jump into the ways that breastfeeding affects your pelvic floor I want to first briefly review some anatomy. If you are pregnant, trying to conceive or postpartum, then I am SURE the internet has bombarded you with information about “Kegels” and “tearing” of the pelvic floor during delivery, but what actually is the pelvic floor?
The pelvic floor is made of a group of muscles that live at the base of your pelvis. Think of your pelvis or hip bones as a bowl, and the pelvic floor muscles are the bottom of that bowl.
www.pelvicglobal.com
Multiple muscles make up 3 layers of the pelvic floor and they all work together with ligaments and other tissue to support the pelvic organs: bladder, uterus and bowel. The pelvic floor plays a huge role in bladder and bowel regulation, sexual function, and core stability — so you could say the pelvic floor is kind of important!
Just like any other muscle of the body (ie. your bicep), your pelvic floor can get weak, tight or overactive.
And this is when many pelvic floor issues come to the surface — hello constipation, pelvic pain, hip pain, leakage!
But did you know that your hormones can also affect the function of the pelvic floor? Let’s briefly look at a few of the big players regarding hormonal health.
Hormonal Changes
Women are no strangers to fluctuating hormones prior to pregnancy, so it is no surprise that there are even more changes that occur during pregnancy and postpartum that can affect your pelvic floor. The big players I want to briefly discuss regarding hormonal health postpartum are estrogen and prolactin.
Estrogen
From a bird’s eye view, estrogen is a sex hormone that plays a large role in female sexual and reproductive health. Estrogen levels are always changing and can vary within each day, month and season of life.
So what happens if estrogen levels are too high or too low?
High estrogen: increased elasticity of your ligaments and tissue, increased vaginal lubrication
Low estrogen: decreased elasticity of your ligaments and tissue, decreased vaginal lubrication
Prolactin
Prolactin is a hormone that plays a role in the formation of breast tissue, lactation and milk supply.
High prolactin: low libido, amenorrhea or irregular periods, discharge of milk from nipples
Low prolactin: decreased milk production
So what happens to your hormones postpartum?
Immediately postpartum, you will have a huge drop in the estrogen hormone coupled with a simultaneous rise in prolactin. The drop in estrogen occurs with the delivery of the placenta as the placenta is one of the major contributors to high estrogen levels during pregnancy. The rise in prolactin occurs with stimulation of your nipple from breastfeeding.
First things first: this is a GOOD thing! Your body has been cranking out higher estrogen levels during your entire pregnancy, because it provides countless benefits to your baby before birth. But after you deliver, estrogen levels go back down, and your body devotes itself to making prolactin, the hormone that produces milk. Again, this is good — it’s exactly what your baby needs! But it can cause unpleasant effects as those two levels change.
How does breastfeeding impact the pelvic floor?
We established that immediately postpartum your estrogen levels will decrease and your prolactin levels will increase in order for your body to start creating milk for your baby. If you choose not to breastfeed, your estrogen and prolactin levels will begin to even out in a few weeks.
If you choose to continue breastfeeding, your prolactin levels will continue to remain high so that your body can continue producing milk. Prolactin blocks estrogen therefore keeping estrogen levels low until your milk supply stabilizes and the frequency of feeds decreases.
So how do these hormonal changes impact the pelvic floor?
Low estrogen levels make you feel like you’re in early menopause causing symptoms such as:
- Decreased vaginal lubrication
- Decreased blood flow to the pelvic floor
- Decreased elasticity of the pelvic floor muscles and tissues
With any or all of the above symptoms you might experience several pelvic floor symptoms such as:
- Itching
- Burning
- UTI-like symptoms (increased urgency and frequency)
- Pain with intercourse
These symptoms can continue for as long as your estrogen levels stay low — which, in many cases, means as long as you’re breastfeeding! In fact, even if you’re not breastfeeding, you may experience these symptoms during postpartum until your hormones return to pre-pregnancy levels.
The good news: you’re not without hope.
Remember, this estrogen drop is temporary. In the meantime, I recommend finding a quality moisturizer for the vulva to prevent dryness — this one’s my favorite, and quality lube for intercourse — I recommend this one to patients all the time.
A couple more ways breastfeeding impacts your body
Not only do the hormonal changes caused by breastfeeding impact the muscles and tissues of the pelvic floor, but they can also impact your libido and menstrual cycle.
Amenorrhea
This medical term simply means the absence of a menstrual period. Low estrogen levels are the cause of this absence, since it’s one of the main hormones that drives a typical cycle. While you’re breastfeeding, you likely won’t see your period return. However, this is more of a “general rule” than an official standard. Every woman’s hormone levels are unique, and some women do get their period while they’re still actively breastfeeding. If you are someone who experiences a return of their period while breastfeeding, don’t be alarmed! This is perfectly fine, and your milk is still absolutely safe for your baby.
Low Libido
Along with your estrogen drop, you’ll also produce less testosterone immediately postpartum. These two hormones are the primary “sex drive” producers, so without them, you might not be in the mood too much. This is also completely normal — in fact, it’s almost like your body’s natural “birth control,” letting you channel hormonal production into prolactin for your current baby before you try to make any new ones. If you’re experiencing a low libido after giving birth, you are not alone. Many women find they need to wait much longer than the “6 week clearance” to return to intercourse for a variety of reasons, including:
- Vaginal dryness caused by low estrogen could make sex uncomfortable.
- Physical exhaustion and bodily changes might mean sex is the last thing on your mind.
- You may not feel the need for oxytocin — it’s normally released during an orgasm, but it also shows up with letdown while breastfeeding. Your body is receiving a form of intimacy through breastfeeding, so it may not feel as imperative to have that need met elsewhere.
What can I do to help?
1. Work with a pelvic floor physical therapist
If pain is keeping you from re-engaging in intercourse with your partner or urinary urgency/leakage is preventing you from engaging in daily activity, a pelvic floor physical therapist can help.
They can help you identify any postpartum pelvic floor issues and provide you with relaxation techniques and exercises.
Click here to find a pelvic floor PT near you!
2. Use lubrication

Uberlube – I recommend this lubrication to my patients on a daily basis. It is silicone-based so it will last longer and will not contribute to dryness as much as a purely water-based lubricant.
3. Use a vulva moisturizer

Vmagic – This product is a GAME changer. Think of it as a lip balm, but for your vulvar tissue. Apply it externally daily and you will notice a significant improvement (both myself and my patients will agree).
4. Invest in my Movement Through Early Postpartum course

In my Movement Through Early Postpartum course you will learn step by step movement sequences to help improve your pelvic floor mobility, improve blood flow to the pelvic floor muscles by appropriately contracting them and connect with your breath to reduce tension in the pelvic floor muscles.
The course also provides you with education for the early postpartum period to control your bladder, types of lubrication, ways to improve intimacy and more!
Remember, these changes are showing up because your body is trying to help you and your baby, not make life harder for you. Hang in there, mama, and know that hormonal balance will come again soon!